Eye Conditions
Hazy Capsule
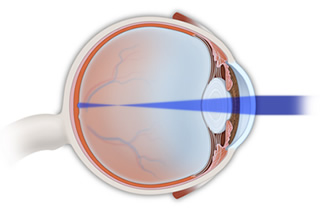
Hazy capsule, otherwise known as posterior capsular opacification (PCO), is the most frequent complication of cataract surgery. This condition affects one out of four patients within five years of undergoing cataract surgery. A hazy capsule is sometimes referred to as a secondary cataract.
During cataract surgery, the clouded lens in the eye is removed from the lens capsule and replaced with a clear, artificial lens called an IOL. Weeks, months or years after the surgery, some patients experience a loss of vision. This sometimes happens because the lens capsule becomes cloudy or wrinkled, blurring the patient’s vision once again.
Symptoms of a hazy capsule are similar to the symptoms experienced with a cataract. They include:
- A gradual decrease of vision
- Vision that is blurry
- Glare around lights
- Sensitivity to sunlight
- Halos around lights
If an examination confirms that this is the case, and if the clouded capsule prevents the patient from functioning, then a posterior capsulotomy may be recommended. This procedure uses a YAG laser to open a window in the back of the lens capsule to restore clear vision. Posterior capsulotomy is a painless outpatient procedure that takes less than 15 minutes. Clearer vision is restored quickly. The improvement of vision depends upon the extent of the clouding experienced and the patient’s eye health. The patient should be able to resume normal activities immediately.
Herpes Simplex
Herpes simplex is a virus that can affect the eyes. It may present with such symptoms as eye redness, watering, sensitivity to light or the feeling that something is in the eye. In some cases, the patient will develop a headache or a rash on the eyelid. If herpes simplex reaches the internal structures of the eye, vision may be compromised. Treatment of herpes simplex will depend upon which portion of the eye is affected, but it often involves antiviral eye drops or oral medication to fight the infection. Corticosteroid drops may also be necessary to reduce swelling or help reduce the risk of scarring.
Herpes Zoster
Herpes zoster, or shingles, is the virus that causes chicken pox. When the body is exposed to herpes zoster, it remains in some of the nerves but is inactive. At times, as we age, something triggers it and causes the herpes zoster to flare up. If a nerve attached to the eye is infected, the result may take the form of a number of eye conditions. Herpes zoster can produce inflammation in several structures of the eye, as well as cause double vision, corneal scarring, glaucoma and cataracts. Treatment often involves taking prescription antiviral eye drops and sometimes corticosteroid drops to reduce swelling or reduce the risk of scarring.
Iritis
Iritis is an inflammation of the iris, which is the colored portion of the eye. The iris is part of a highly vascularized fibrous tissue called the uvea. This condition frequently manifests in young to middle-aged individuals and may only affect one eye. Iritis may be caused by trauma to the eye, an infection or the effects of certain diseases.
The symptoms usually develop quite quickly and unexpectedly, but in some individuals they form slowly. Distinguishing symptoms of iritis may include:
- Irritation and redness of the eye
- Eye pain
- Sensitivity to light
- Blurred vision
A diagnosis of iritis typically takes place after a physical examination of the eye, during which your doctor will use a special microscope called a slit lamp to obtain a magnified view of the eye’s structures.
To treat iritis, the patient will be encouraged to wear dark glasses and take pupil dilating drops to relieve pain and pressure. Serious cases usually require extended use of steroid eye drops as well as oral steroids that suppress the immune system. When iritis results from an underlying condition such as herpes, AIDS or syphilis, the disease may need to be treated to see improvement in the eye. Iritis may become a chronic problem.
Keratoconus
Keratoconus is a progressive eye disease in which the normally round cornea thins and begins to bulge into a cone-like shape. The resulting irregular, cone-shaped cornea deflects light, causing distorted vision. Treatment of keratoconus may involve fitting the eyes with rigid gas permeable (RGP) contact lenses or in more severe cases, corneal transplant surgery.
Macular Degeneration
Macular degeneration, also known as age-related macular degeneration (AMD), is a common condition in older adults and the leading cause of vision loss and blindness in people over the age of 65. Macular degeneration affects the macula, the part of the retina responsible for the crisp, detailed vision needed for reading or driving. In individuals with AMD, the tissue in the eye responsible for central vision slowly begins to deteriorate, which can significantly affect a patient’s quality of life.
Nearsightedness
 Myopia, also known as nearsightedness or shortsightedness, is a condition of the eyes in which nearby objects are clear and distant objects appear blurry. Almost a third of people in the United States experience some degree of nearsightedness.
Myopia, also known as nearsightedness or shortsightedness, is a condition of the eyes in which nearby objects are clear and distant objects appear blurry. Almost a third of people in the United States experience some degree of nearsightedness.
Myopia may be caused by some of the following:
- Excess corneal curvature
- An oblong shape to the eye
- A family history
Symptoms include difficulty focusing on objects in the distance, such as a chalkboard or TV. Other signs of myopia include some of the following:
- Difficulty seeing objects in the distance
- Squinting
- Eye strain
- Headaches
- Fatigue
- Excessive blinking
- Rubbing eyes
Eyeglasses and contact lenses are common methods of correcting nearsightedness. Eyewear may be used for certain activities, like watching television or driving, or for all activities. Surgical options for the correction of myopia include vision correction procedures such as refractive and laser surgery.